Once a notoriously sight-robbing disease, wet AMD is now becoming a controllable condition.
By Susan K. Treiman
Medically Reviewed by Laura J Martin, MD
Reviewed: November 30, 2021
When the U.S. Food and Drug Administration (FDA) approved Susvimo, a revolutionary new treatment system for wet age-related macular generation (wet AMD) in October, it marked the biggest breakthrough in the 15 years since the injectable blood vessel growth inhibitor Lucentis transformed this once untreatable condition into a manageable one.
It won’t be the last. Researchers are working on a number of innovative approaches to assist the 11 million Americans with some form of AMD. Several of the most dramatic developments target the devastation caused by the wet, or advanced, stage of the progressive disease: Implanted devices, novel drug delivery systems that use retinal genes, stem cell applications, and therapy formulations that lengthen the time between treatments are all being pursued.
“We’re now entering a second age of wet AMD treatments,” says Peter A. Campochiaro, MD, the George S. and Dolores Doré Eccles Professor of Ophthalmology and Neuroscience at the Wilmer Eye Institute of Johns Hopkins Medicine, headquartered in Baltimore.
Dr. Campochiaro, a leading expert on AMD, macular disorders, and diabetic retinopathy, added that, for a health problem projected to affect 22 million Americans by mid-century, the advances are coming just in time. “The need for new options is urgent,” he says.
AMD: Complex Causes Yield Insight Into Treatments
AMD is complicated, and its causes are likely multifactorial. “So far we know it’s about inadequate blood vessels, cell damage from free radicals (unstable molecules produced by the body’s metabolic processes and environmental stressors), and the immune system actually attacking the retina,” says Joshua Dunaief, MD, PhD, the Adele Niessen Professor of Ophthalmology at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia.
“Inflammation plays a role in AMD, and so do lipids (blood fats) and possibly iron toxicity,” Dr. Dunaief adds. “Plus, blood levels of C-reactive protein, an indicator of inflammation, tend to test high in people with wet AMD. That suggests that general inflammation might be involved.”
Experts are actively exploring the inflammatory aspect of the disease for treatments. Researchers are also deep diving into what’s already known about the wet AMD dietary connection. Dunaief, along with his brother David Dunaief, MD, an internist specializing in integrative medicine, are among the researchers whose work, such as a study published in December 2019 in the American Journal of Lifestyle Medicine, shows that a plant-rich diet can rapidly lower the levels of C-reactive protein, which, theoretically, could decrease AMD risk.
VEGF Produces the First Innovations
Normally, a signaling protein called vascular endothelial growth factor (VEGF) helps heal wounds by dispatching extra blood and oxygen to an injury site. But in people with AMD, blood vessels haphazardly proliferate in a part of the retina where they shouldn’t be, kick-started into chaotic growth by VEGF. Fragile and unstable, these blood vessels eventually leak blood that scars the retina and compromises vision. When this happens, dry AMD has effectively become wet AMD.
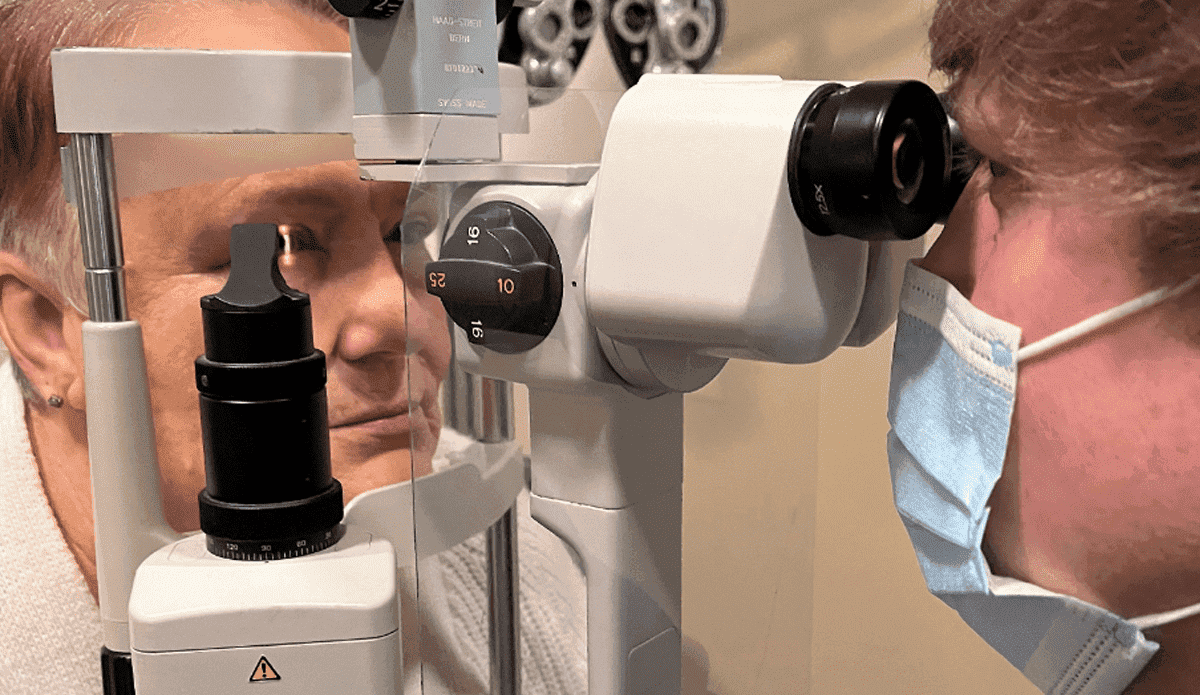
In 2006, the FDA approved a new drug, Lucentis, that halts unstable blood vessel growth. The medication, which is injected monthly into the fluid-filled center of the eye, is capable of stopping the destruction and has effectively transformed what was previously the leading cause of blindness among older people into a chronic but controllable medical condition.
Today, vascular endothelial growth factor antagonists are the wet AMD treatment standard. These VEGF-A drug injections include the following:
- Lucentis (ranibizumab) The Roche Pharmaceutical in-the-eye injection became the first FDA-approved drug for wet AMD in 2006. It’s administered once a month for at least the first year.
- Eylea (aflibercept) A Regeneron Pharmaceuticals product, Eylea is also injected into the eye for the first three months, then every two months.
- Avastin (bevacizumab) Produced by Genentech, Avastin is injected into the eye every four to six weeks as a liquid administered slowly into a vein.
- Beovu (brolucizumab-dbll) Beovu, made by Novartis, is injected into the eye monthly for the first three months, then once every 8 to 12 weeks.
Despite their extraordinary success, VEGF-A drug treatments have been dogged by patient noncompliance, primarily because of obstacles to care.
“We’ve learned that the results in clinical practice are not nearly as good as they can be, because it’s difficult to maintain the frequency of injections if you’re older or disabled,” Campochiaro says. “Things get in the way. And every time a patient misses an appointment the disease returns.”
Several research efforts are taking aim at that challenge.
On the Horizon: Breakthrough Therapies, Novel Approaches
Newer therapies are venturing beyond VEGF-A drugs. Among them:
A port delivery system to replace injections The FDA’s October 2021 approval of Genentech’s Susvimo (previously called port delivery system with ranibizumab) represents the first use of an implantable device to treat an internal eye problem. Clinical trials described in Ophthalmology in September 2021 yielded a 98 percent success rate, with benefits identical to those of the monthly injections.
The therapy begins with a one-time surgery to permanently stitch a tiny device, roughly the size of a grain of rice, under the white, outer portion of the eye in an area hidden beneath the lid. The device regularly releases small doses of a customized formulation of Susvimo for six months. After that, the patient returns twice a year for a medication “fill-up” using a special syringe.
“The results show that it replaces the injections and, more importantly, doesn’t sacrifice anything in the process,” says Peter Kaiser, MD, a professor of ophthalmology at the Cleveland Clinic in Ohio. “So, we’re getting as good a result as before; probably a better one, because this is a long-term therapy.”
The drug, however, carries a black box warning of a vastly increased risk of endophthalmitis, a severe eye infection considered a medical emergency that requires immediate attention. Still, its recent approval means that it will likely reach many more ophthalmologists during 2022.
Longer-lasting drugs The Roche drug faricimab, now awaiting FDA approval, is a quarterly injection of a bispecific antibody that blocks both VEGF and the protein angiopoietin-2, another trigger for the blood vessel permeability that leads to wet AMD. Also in development are Abbvie and Molecular Partners’ abicipar pegol, which lasts for three months, and sunitinib by Graybug Vision, potentially a six-month treatment, both of which are also intended to inhibit blood vessel growth.
Gene therapy Retinal gene therapy harnesses an altered, harmless, adeno-associated virus (AAV) that is placed in the eye via injection or during an operating room procedure. Once implanted, the gene coaxes the retina into manufacturing its own VEGF-A-blocking protein. The treatment is intended to be a “one and done” intervention for wet AMD, with the body indefinitely bathing the eye in its own anti-VEGF proteins generated by the altered gene. So far, the results are promising.
“It’s now in phase 3 trials, with data out to three years that show patients do continue to produce the therapeutic protein,” says Campochiaro. The general concern about gene therapy is that the genetic changes can last forever with unknown consequences. Because of that, the ongoing effect of these genes needs to be carefully addressed in clinical trials to confirm their long-term safety.
Vitamin and nutritional therapies Today, some enhanced fish oils and AREDS 1 and 2 (age-related eye disease study) vitamins — formulated with zinc, lutein, zeaxanthin, and other substances — are widely used as tablets to slow dry AMD. Although they’re believed effective, a study published in December 2020 Oxidative Medicine and Cellular Longevity cautioned that the supplement didn’t entirely block intermediate AMD progression over an eight-year period. Other dietary connections may offer additional nutritional treatment opportunities, given the known links between wet AMD, a Western type diet, and other systemic conditions, Dunaief says. In a 2018 report published in Ophthalmology, researchers found that sticking to a diet rich in healthful nutrient-rich foods such as fruits, vegetables, legumes, and fish reduced the risk of progression to advanced AMD by 41 percent among the more than 4,000 participants (all over 55).
RELATED: Managing Wet AMD: 8 Key Nutrients to Include in Your Diet
Further Down the Line: AMD Possibilities, Not Yet Probabilities
Stem cell treatments Stem cells, too, may one day help regenerate damaged portions of the retina. These immature and undifferentiated cells don’t yet have an assigned function in the body, so they can assume many forms, including that of retinal cells. The stem cells can originate in fetal or adult cells. Still problematic, though, are the potential sources for the stem cells used therapeutically, which are currently too unreliable (an individual’s own skin) or too controversial (from an aborted fetus).
Scientists continue to seek ways to harvest immature cells from a patient’s own body to replace those damaged by wet AMD. “There have been some early successes where patients have received stem cell inserts and the retina has gone on to produce those cells, but it’s phase 1 data and we still have a lot to learn,” says Dr. Kaiser at the Cleveland Clinic.
Eye drops British researchers are testing eye drops that could deliver results similar to those achieved by regular injections. Reporting in the May 2017 Investigative Ophthalmology & Visual Science journal, they said that they detected evidence of the anti-VEGF eye drop in the eyes of mice within six minutes of application. Still unknown, though, is what that can mean for human beings. “I’m hoping drops will be effective someday,” says Dunaief, “but it’s difficult to get active ingredients to the retina at the back of the human eye.”
Pills and tablets Research published online in JAMA Ophthalmology in July 2017 referenced a study in which participants received VEGF-A blocking pills for 24 weeks. Sixty percent of the 25 trial participants said they required no additional anti-VEGF injections afterward. Early trials were stopped when some patients were found to have gastrointestinal and liver problems. The study concluded that the limited tolerability and safety argued against further investigation at the time.
Up Next: Biomarkers to Help Researchers Predict and Track the Course of the Disease
With the current research possibilities exploding, the best basic information for future innovations may come from a major National Institutes of Health (NIH)/National Eye Institute study tracking 500 AMD patients for five years. The study’s goal is to identify biomarkers of disease progression well before the degeneration advances to late-stage disease and causes vision loss.
As research continues, it’s a high-stakes race, but one in which additional victories are likely imminent. Those successes would further change AMD from a potential vision thief to a condition with controllable, even reversible, outcomes.
“When I started treating people, just about 21 years ago, there wasn’t much we could do to slow vision loss beyond photodynamic (laser) therapy,” Dunaief says. “Now that we can stop it, we’re looking for better ways to do that.”






